Gingivostomatitis in Cats - Causes and Treatment



See files for Cats
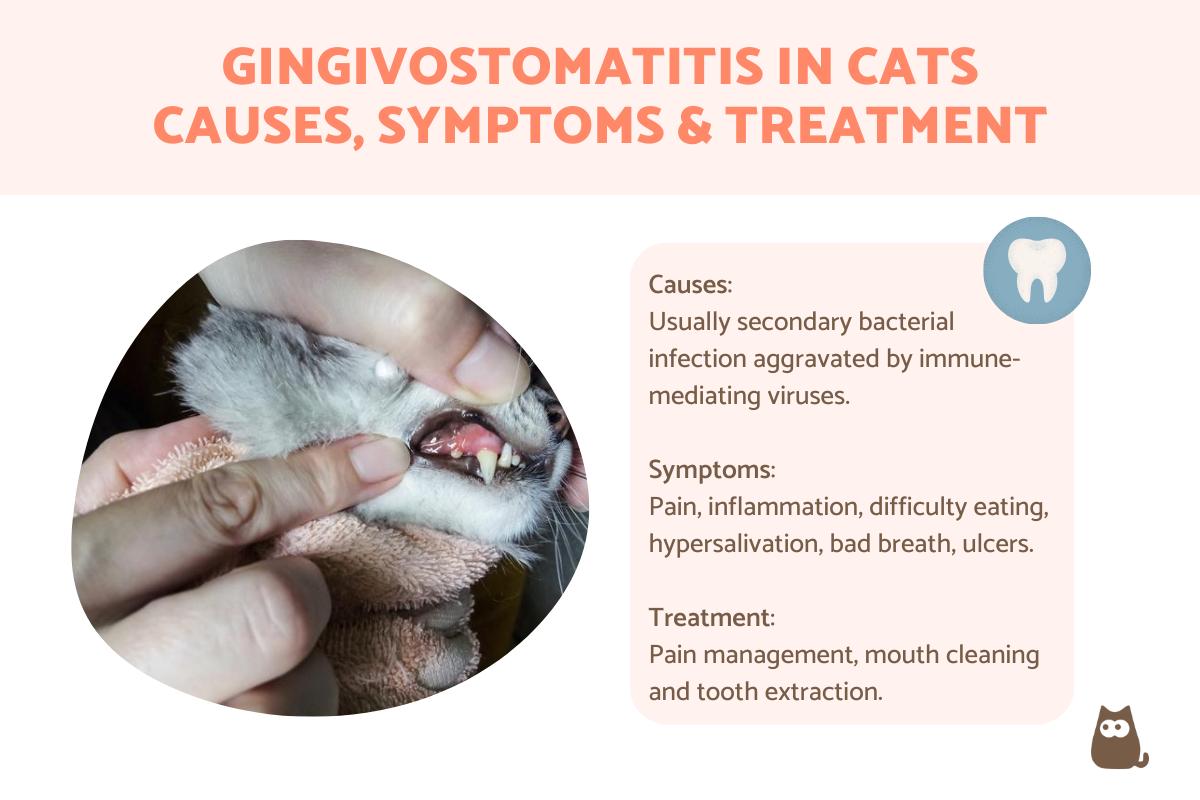
When a cat has swollen and red gums, guardians often first notice it due to the cat's bad breath. This is because the inflammation is linked to bacteria in the mouth which is often accompanied by plaque and tartar buildup. While painful and stressful on their own, they can cause serious repercussions since they can prevent the cat eating and threaten their overall health. The risk of sepsis due to the infection entering the bloodstream is another cause for concern. For localized inflammation to the gums (gingiva), we can see gingivitis. However, when there is inflammation then spreads throughout the oral cavity, gingivostomatitis can appear. This is especially related to immune-mediated factors.
At AnimalWised, we find out about gingivostomatitis in cats by looking at the causes, symptoms and treatment feline gum inflammation.
What is gingivostomatitis in cats?
Gingivostomatitis is a chronic condition which is relatively common in cats. It consists of an extensive inflammation around the cat's mouth that includes the gingiva and lasts longer than six months. Stomatitis is an extensive inflammation of the oral mucosa that excepts the gingiva and can be acute or chronic. Gingivostomatitis includes the gingiva and is almost always chronic.
In addition to the gums, the inflammation accompanying gingivostomatitis in cats can affect the tongue, soft palate and other oral mucosa. It normally affects adult cats and is rare in kittens. Although there is little research to support breed disposition, it is anecdotally more prevalent in Siamese, Persian, Burmese and Himalayan cat breeds.
This periodontal disease in cats can be mild, moderate or severe, usually also presenting with some level of ulceration. Once of the conditions that characterize this pathology is caudal stomatitis, an inflammation of the deepest part of the mouth. It can sometimes be proliferative, meaning it can also affect the tongue.
Feline gingivostomatitis is sometimes referred to by other names. It has been alternatively known as feline ulcerative-proliferative gingivitis, chronic gingivitis-stomatitis-faucitis, caudal stomatitis, plasmacytic pharyngitis stomatitis, chronic gingivitis-pharyngitis, plasmacytic lymphocytic stomatitis gingivitis and chronic stomatitis.
Causes of chronic gingivostomatitis in cats
This disease has been linked to a chronic infection with feline calicivirus. This is because around 70% of cats diagnosed with gingivostomatitis have also tested positive for this virus, although not all. It is important to note that treatment for the gingivostomatitis can reduce inflammation without decreasing the viral load.
In this way, feline gingivostomatitis is linked to lowered immunity which predisposes the cat to secondary bacterial infection. The feline calicivirus can encourage the entry of other pathogens by damaging cell membranes. In this way, it is not a direct cause of gingivostomatitis in cats, but an aggravating factor. Feline retroviruses such as feline leukemia virus or feline immunodeficiency virus can can also increase the proinflammatory response.
Stress reduces immunity. In homes with several cats or colonies with multiple cats living in close contact there is an increased risk of developing chronic gingivostomatitis. This is due to greater contagion of predisposing or aggravating feline viruses.
The most accepted cause is of immune-mediated origin, with an exaggerated reaction of the immune system and an alteration in the local immunity of feline saliva. Although cats with chronic gingivostomatitis have an increase in immunoglobulin A (IgA) in serum, it has low levels in saliva. IgA is responsible for interfering with bacterial adhesion and neutralizing pathogens and toxins released by bacteria in the oral cavity.
The oral antigens related to the overreaction of the immune system are:
- Bacterial plaque (most often Pasteurella multocida)
- Periodontal disease
- Feline tooth resorption by the action of odontoclasts
- Food allergens
Learn more about oral health issues in felines with our article explaining why cats have yellow teeth.

Symptoms of gingivostomatitis in cats
The clinical signs presented by a cat with chronic gingivostomatitis are not only limited to the oral cavity. The pain caused by the process makes them have difficulty in eating with consequent weight loss. This is exacerbated when they have problems swallowing (dysphagia). Oral pain causes them not to groom themselves, causing their hair to have poor conditioning.
Feline chronic gingivostomatitis is also characterized by presenting the following symptoms:
- Ptyalism (hypersalivation)
- Halitosis (bad breath)
- Oral bleeding
- Ulcers in the oral mucosa
- Lip or oral stomatitis
- Caudal stomatitis
Caudal stomatitis is sometimes accompanied by glossopharyngitis and granulation tissue in the caudal oropharynx. Granulation tissue is the new tissue that presents when the oral mucosa repairs itself.
Discover more about why a cat has hypersalivation in our article on why a cat keeps drooling.
Diagnosis of gingivostomatitis in cats
The first thing to do when we observe the signs of gingivostomatitis in cats is to go to a veterinarian. There are other oral health conditions which share some of these symptoms, so it is important for a differential diagnosis to be carried out. This will rule out the following potential health issues:
- Feline eosinophilic granuloma complex
- Oral tumors
- Trauma
- Irritation due to ingestion of corrosive substances
- Other periodontal disease
- Pemphigus
- Systemic lupus erythematosus
- Uremic mouth ulcers due to kidney failure
- Diabetes mellitus
- Hypervitaminosis A
- Feline immunodeficiency infection or severe feline leukemia
To do this, a series of diagnostic tests must be applied to identify the antigenic stimuli responsible for the immune-mediated response, as well as rule out the aforementioned diseases. The following diagnostic tests will be carried out:
- Calicivirus PCR test
- Tests to rule out feline leukemia and immunodeficiency
- Dental x-ray to assess the condition of the teeth and detect periodontal disease or tooth resorption
- Biopsies of affected tissue for histopathological analysis
- Bacterial culture to determine the predominant bacterial flora and antibiogram
Biopsies are used to determine ulcerated mucosal tissue with a dense inflammatory infiltrate in the submucosa with a predominance of plasma cells, lymphocytes, histiocytes and neutrophils. They are mainly used to rule out tumors such as oral squamous cell carcinoma in cat's mouth.
If feline gingivostomatitis is confirmed, the blood and biochemistry analysis will show an increase in immunoglobulins, mild anemia, an increase in white blood cells with neutrophilia (increased neutrophils) or eosinophilia (increased eosinophils). Some cats may also present lymphopenia (decreased lymphocyte count). Around 10% of cats with chronic gingivostomatitis have concurrent kidney disease, with altered kidney parameters seen.
Learn about polycystic kidney disease in cats with our related guide.

Gingivostomatitis in cats treatment
It should be noted that chronic gingivostomatitis in cats is difficult to treat. Therapies are aimed at managing symptoms by reducing plaque buildup, treating dental disease and controlling inflammation.
The treatment of feline gingivostomatitis will consist of:
- Analgesics in the form of opioids such as buprenorphine and NSAIDs such as meloxicam
- Plaque removal by daily brushing with chlorhexidine (after pain subsides)
- Clindamycin is an effective antibiotic for gingivostomatitis in cats when confirmed by antibiogram
- Mouth cleaning
- Rinse in water with chlorhexidine or apply adhesive gels with this active ingredient
- Change to a hypoallergenic or another novel diet
Despite being useful for reducing inflammation, corticosteroids are not effective. They increase the viral load by causing immunosuppression and are necessary in increasingly higher doses.
In mild or moderate cases, an extraction of teeth affected by periodontal disease or feline dental resorption can be performed. In more serious cases of chronic gingivostomatitis or if improvement does not occur with the above treatment options, an extraction of all molar and premolar teeth. This extraction is considered the best therapy for this disease, curing 50-60% of cats.
Some cats are not completely cured after extraction, but their pain and inflammation are reduced, allowing them to eat again. In a very low percentage they will remain the same, but mesenchymal stem cells or omega interferon can be used, whether positive or negative for feline calicivirus. This generally provides good results.
In addition to gingivostomatitis in cats, learn about other reasons why a cat's breath stinks do bad.
This article is purely informative. AnimalWised does not have the authority to prescribe any veterinary treatment or create a diagnosis. We invite you to take your pet to the veterinarian if they are suffering from any condition or pain.
If you want to read similar articles to Gingivostomatitis in Cats - Causes and Treatment, we recommend you visit our Other health problems category.
- V. Aybar, J. Vega. (2011). Diagnostic and therapeutic protocol for feline chronic gingivostomatitis.
https://avepa.org/pdf/boletines/Medicina_Felina_Boletin5.pdf - ML Palmero. Feline chronic gingivostomatitis. https://www.gattos.net/images/Publicaciones/Marisa/ArticulosNuevos/17AGingivoestomatitiscronicafelina.pdf
- A. Lloret. Feline chronic gingivostomatitis (GECF): Pathogenesis. https://www.congresoveterinarioibiza.com/wp-content/uploads/Mesa-redonda-gingivostomatitis-pathogenia.-A.-Lloret.pdf